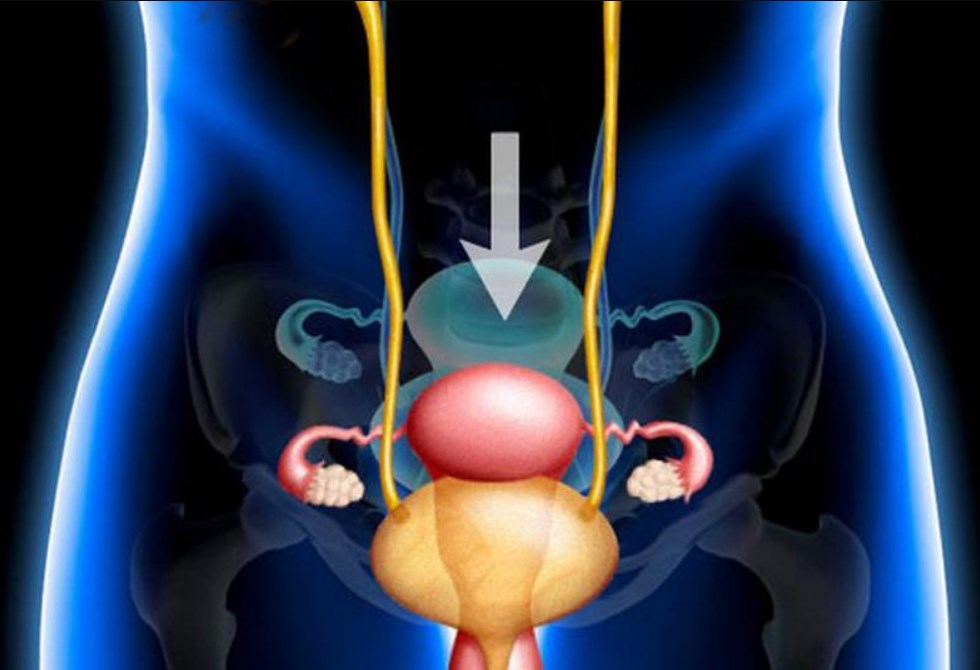
Bladder Prolapse
It is the displacement of the bladder downwards from its normal position. It occurs as a result of the weakening of the pelvic floor muscles. Bladder prolapse It usually occurs due to reasons such as birth, aging or heavy lifting. Urinary incontinence, frequent urination and a feeling of fullness in the vaginal area may be observed. If left untreated, complaints increase. It can be corrected with physical therapy or surgical methods. It is more common in women.
What are the symptoms of bladder prolapse?
A persistent feeling of fullness or pressure may occur in the lower abdomen or vagina. It is possible to feel or see tissue or a mass coming out of the vagina. Difficulty urinating, a feeling that the bladder is not completely empty, or the urine stream is intermittent. Urinary incontinence may occur when coughing, sneezing, laughing, or lifting heavy objects.
There may be a need to urinate frequently throughout the day and night. There may be pain or discomfort during sexual intercourse. There may be widespread and constant pain in the lower back. Frequent urinary tract infections occur because the bladder does not empty completely, causing bacteria to grow. Pressure in the pelvic area can affect bowel movements. Bladder prolapse If your symptoms become severe, it is important to see a urologist.. Early diagnosis and appropriate treatment can prevent its progression.
What Causes Bladder Prolapse?
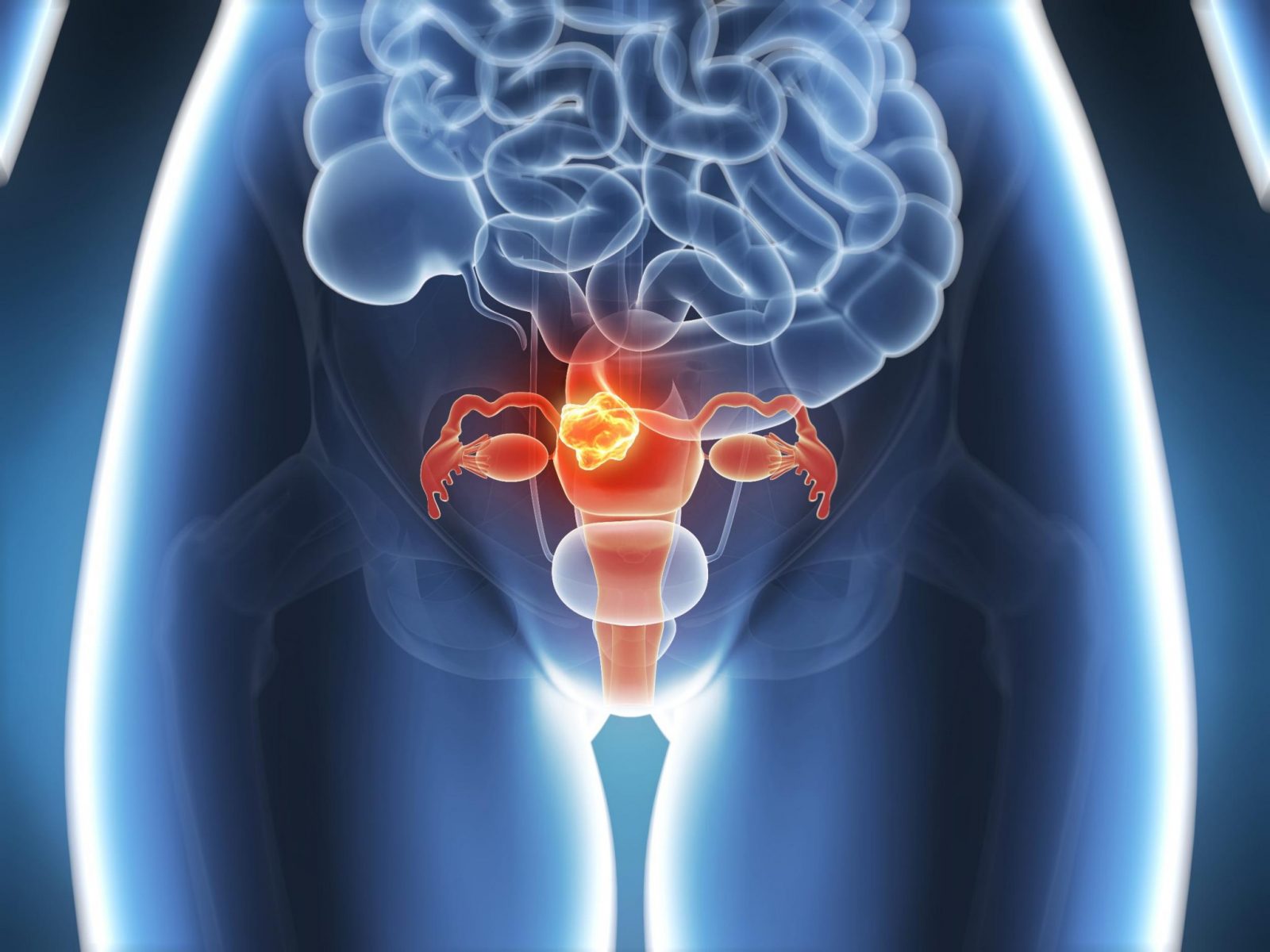
Difficult or multiple vaginal births can cause the pelvic muscles to weaken. Pelvic floor muscles can lose strength with age. Constantly lifting heavy loads can put pressure on the pelvic area. Prolonged coughing can increase intra-abdominal pressure, bladder prolapse can cause. Excess weight puts additional pressure on the pelvic floor muscles and weakens them. The decrease in estrogen hormone causes the tissues in the pelvic area to weaken. Prolonged straining can put pressure on the pelvic muscles and cause the bladder to sag. Operations such as hysterectomy can weaken the support structure of the bladder.
How Is Bladder Prolapse Diagnosed?
The doctor listens to the patient's complaints and takes a detailed medical history. Typical symptoms include urinary incontinence, a feeling of pressure in the pelvic area, and swelling in the vagina. During the gynecological examination, the vagina and pelvic area are checked for any prolapse. The patient is asked to cough or strain. bladder prolapse presence and degree are assessed. Pelvic ultrasound allows visualization of the bladder and surrounding tissues. The degree of bladder prolapse towards the vagina can be determined. Urodynamic tests are used to evaluate urine flow and bladder capacity. These tests are important to determine dysfunctions due to prolapse.
Pelvic MRI provides detailed visualization of soft tissues and can assess the severity of prolapse. It is especially preferred in advanced prolapses. Cystoscopy is the imaging of the inside of the bladder through a thin tube. It is used to determine if there are other abnormalities in the bladder wall or urinary tract. The pelvic organ prolapse grading system determines the severity of prolapse. It is a systematic classification. Evaluation is made from Stage 1 (mild) to Stage 4 (advanced). After diagnosis, bladder prolapse An appropriate treatment plan is created depending on the severity of the condition.
What are the Treatment Methods for Bladder Prolapse?

Pelvic floor exercises (Kegel Exercises) strengthen the pelvic muscles. Helps to correct mild sagging. Avoiding excessive weight, avoiding heavy lifting and preventing constipation support the treatment. Vaginal tissues can be strengthened with estrogen supplements, especially after menopause. Special physical therapy methods that strengthen the pelvic muscles can be applied. Surgical operations are preferred to support the bladder in advanced sagging. The treatment method, bladder prolapse is determined according to the degree of the disease and the general health status of the patient.